Working with trauma as the central issue of our work means that we must understand the dynamics and processes of trauma, including the phenomenon known as re-traumatisation. Because as practitioners of a therapy that centralises trauma, re-traumatisation in our work will happen, and we need to know exactly what we are talking about, and as practitioners what is required of us in that moment.
So this essay sets out to do four things:
- Define as exactly as I can what re-traumatisation is;
- Then understand its place in our work with trauma;
- Look at our attitudes towards re-traumatisation;
- Decide on ways of managing it when it happens to the benefit of the re-traumatised person;
- Look at some of the reasons why a re-traumatisation might happen in our work.
What exactly is re-traumatisation? We use the term perhaps far too easily and far too often; in the same way as the usage of the words ‘trauma’ and 'abuse' have proliferated without a clear definition of what we are talking about.
I should say at this point that most of what I am setting out on this topic is what I have developed in my thinking from 30 years or so as a psychotherapist and 12 years of immersing myself in the psychotrauma theory and therapy developed by Franz Ruppert as Identity-oriented Psychotrauma Therapy (IoPT). I cannot find much else written that is useful on the topic... So please regard this as a work in progress, and feel free to share your own thoughts and experiences through the comments section at the end of the blog. Perhaps together we can develop an understanding of re-traumatisation that allows practitioners to work with trauma with increased confidence and stability. It is quite a long article, because once I got started all sorts of half-formed thoughts and understandings from my experience emerged.
So for starters let’s briefly re-cap what we mean when we use the term ‘trauma’ in IoPT thinking.
What is Trauma?
Trauma is:
- A situation where the person traumatised is utterly helpless and overwhelmed by the forces at play… in relational trauma (as opposed to natural traumas such as earthquakes or floods etc) this means that one person, the ‘perpetrator’, holds all the power and the other, the ‘victim’, holds none.
- High stress resources and strategies – ‘fight and flight’ – are not possible… because if one could fight or flee one is not actually helpless.
- The situation is experienced as a life and death situation: the person’s experience is as if they might die, in the moment their very survival is in the balance.
- The psycho-physical system has to split in order to manage the experience. The splitting in the first instance is a dissociation from the unbearable experience of reality, and this then over time becomes an increasingly structural and reified split. This split is best shown in the symbol shown below.
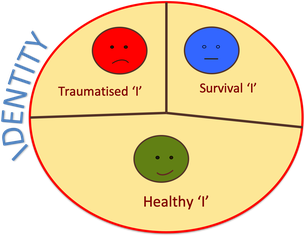
The ‘survival self’ is a trauma survival part of the psyche, the sole function of which is to protect the person from the split off trauma experience, to keep it out of daily consciousness. This trauma experience at the time of traumatisation is in fact barely experienced; it is cut off before the full experience and emotional discharge can happen.
It then sits as an unprocessed and unfulfilled element in the psycho-physical system; it cannot be metabolised, but like the proverbial elephant in the room it is always there.
The Psycho-Physical
It is important to realise that the trauma experience is an experience of the psyche (the mind and emotions) and the physical, the body. While a trauma may from the point of view of an external observer look more like a physical trauma, for example a physically violent assault, or like a psychological trauma, for example the neglectful and unloving attitude of a mother, all traumas happen in the totality of the body-mind, and the splitting that happens is also a mind-body splitting. So body-workers who are sensitive to body states will find that one part of the body is numb, or particularly tense, held, unresponsive to treatment etc.
The Split Processes
So the first step in understanding re-traumatisation is to realise that there is always an internal conflict process within the person: the trauma experience consistently urges for completion by being experienced and allowed its full expression, while the ‘survival part’s’ entire purpose and function is to avoid that. The ‘healthy self’ always also urges for wholeness, for completion… that is what health is, and in this sense the ‘healthy self’ is also in conflict with the ‘survival self’, but at the same time this part can only really function as a healthy element in the moment because the ‘survival self’ holds the split. For day-to-day functioning the ‘healthy self’ needs the ‘survival self’ to protect it from being overwhelmed by the unresolved trauma experience…
So from this understanding our first principle of defining what re-traumatisation is could be:
The failure of the survival self to be able to hold the boundary and protect the healthy self from being overwhelmed by the un-metabolised trauma experience.
Daily life
Our daily life is a constant process of the relationship between these three different elements of ourselves as we navigate through the tensions and stresses of our day.
Our physical senses are our main organs of contact with our world: hearing, sight, smell, touch, taste. These are the ways in which we experience our world, while our internal processing of this information, and the meaning we then make of it is influenced by how we perceive it.
Our perception, and thence our reaction to our world, is influenced by many, many things including accumulated prejudices, biases, the nature of our early relationships, our trauma of identity and our ability to feel and be loved by our parents or not – in effect our distortions of reality that have accumulated over our life’s experience.
And our reactions to this sensory information are in the form of our emotions… anger, joy, grief, love, fear, terror, sadness. Our actions in life always come from our emotional response to sensory perception… but these emotional responses are always influenced by the processing relationship between the ‘survival self’, the ‘trauma self’ and the ‘healthy self’, ie from our trauma. It is perhaps shocking to realise that all of our decisions in life, even those we think are purely rational, all come primarily from our emotional (gut response) reactions to our perception and our internal distortions of reality which are the result of trauma.
So for a severely traumatised person whose ‘survival self’ has taken the route of rigid control, and pretty much banished or hardened the boundaries against those emotions that leave one feeling vulnerable, such as love, compassion, joy etc, for fear that experiencing these emotions will allow the trauma emotions to emerge, their reactions to most external events will likely be aggressive, loveless and lacking in empathy and compassion.
Chaos and Rigidity as survival forms
It is worth mentioning here two distinct forms of trauma survival patterns, defined by Dan Siegel (clinical Professor of Psychiatry ad UCLA and Director of the Mindsight Institute) as rigidity and chaos.
How I understand this in IoPT terms is that, depending on the contextual possibilities (our family culture) when we are babies in relation to our trauma survival, our patterns of trauma survival tend towards either a more rigid, controlling form, or a more chaotic and uncontrolled form, and in some people there is an oscillation between rigidity and chaos.
The rigid form requires a high degree of control and desensitisation to keep the trauma out of consciousness, whereas the chaotic form is uncontrolled and instead uses emotionality and chaotic behaviour as a way of distraction from the trauma. The more rigid form allows little real emotion whereas the more chaotic form uses ‘survival emotions’ to defend against the real emotions of the trauma.
Limbic Resonance
Another form of our connection with the external world comes primarily from our limbic brain system: it seems that we are much more in unconscious connection with each other than we realise through what is known as ‘limbic resonance’ (Lewis, Amini and Lannon. 2001).
In the initial attachment process between mother and child the limbic brain (also known as the mammalian brain) of both mother and child enables them to communicate, resonate and synchronise with each other for the safety and survival of the child. This ability to resonate less consciously with those around us continues into adulthood, and underlies the representative experience in the Intention Method that we use in IoPT to understand our trauma.
So it is likely that some of the information we perceive from our environment is due to our limbic resonance ability.
Mirror Neurons
Mirror neurons (Rizzolatti & Craighero, 2004) are also a significant way in which we are continually in contact with those around us. The mirror neuron effect is well encapsulated in the following quote:
“We have all experienced moments in which we find ourselves moved – not because of what happened to us, but because of what happened to someone else.” (Keysers, 2011 in Broughton, 2013)
Mirror neurons allow us to empathise with the experience of others by feeling it as if it were happening to us. It is mirror neurons that make books, films and theatre so successful… we feel what is shown us as if it were happening to ourselves, we are emotionally awakened in resonance with the story being told. For many people who have suppressed so much of their emotional life in the management of their trauma, the ability to resonate with a film or other story is a way of feeling more alive in themselves... for a while.
However, these myriad ways in which we live in our world are also the ways in which our split off trauma is likely to be re-triggered.
What is the re-triggering of trauma?
Exactly as stated above: it is the sensory, semi-conscious and unconscious perceptions of our world that can also be the triggers to a re-experiencing of our trauma. The potential for our traumas to be re-stimulated is possible in every moment of our lives, in every encounter with others, and for the most part happens unconsciously.
Most often however these re-triggerings are successfully dealt with by our trauma survival strategies, the many daily strategies developed by our survival self to deal with exactly these situations. We may not even notice the process; or we may have developed sufficient self-awareness and recognition of our survival strategies to be able to realise we have gone into survival, and even to be able to ask ourselves the question: What happened that I have gone into my survival strategies?
However, on occasion the re-triggering may be more serious than this, and for a while we can feel quite disoriented, depressed, anxious, emotional or disturbed without really understanding why... perhaps we might say we are having a bad day or are feeling out of sorts or down in the dumps. This is a more severe re-triggering that the survival self may struggle to control. As long as the survival strategies manage to control the trauma and keep it out of full consciousness this will stay in the realm of re-triggering. However if the survival part of ourselves fails in this then we are into a full re-traumatisation.
So what then is re-traumatisation?
We now arrive at the central topic of this blog piece, and an attempt at a definition of exactly what re-traumatisation is. We have our first principle, stated above, as:
Re-traumatisation is the failure of the survival self to be able to hold the boundary and protect the healthy self from being overwhelmed by the un-metabolised trauma experiences.
In this sense it is more than a re-triggering of one’s unresolved trauma; it is a re-triggering that the survival self is unable to control which then progresses into a full re-traumatisation.
There are two possible outcomes of such an event:
- The first is that the psyche dissociates and splits again as way of managing the experience as if it were a new traumatisation, resulting in further splits in the psyche. It is important to note here that all traumatic events after one’s original trauma are always a re-stimulation of that original trauma (most likely a Trauma of Identity) in addition to the burden of the current trauma event. It is that first trauma experience that influences our ability to manage later events that may or may not be experienced as traumatic.
- The second is a full-blown experiencing of the original feeling of helplessness, panic and emotions involved that have been suppressed and split off into the unconscious.
In the second instance there are another two possibilities:
- The experience is a repeat of the original experience, where the person loses contact with the here and now reality and internally is transported back to the original event as if it were happening now, with no sense of contact with the present. This is an unhelpful repetition of the traumatisation.
- The person stays in contact with the here and now reality at the same time as experiencing the previously suppressed emotions. The experience then can be a healthy expression within a safe and supportive environment. I consider this potentially a transformative and healing experience.
In the second possibility I want to refer to the work of Ernest Rossi who worked closely with Milton Erikson of the hypnotherapy tradition. I read a book of his back in the 1990s in which he talked about ‘state-dependent memory’ (Cheek, David B. & Rossi, E., 1995).
State-dependent memory is
“…the phenomenon through which memory retrieval is most efficient when an individual is in the same state of consciousness as they were when the memory was formed.” (Wikipedia)
State-dependent memory as Rossi discussed it (not, I must add, in relation to trauma particularly), is the way in which our memory system takes a sensory snapshot of the situation, ie capturing whatever the sensory information is at the time… smell, imagery, auditory, tactile etc. This is the ‘state of consciousness’ of the event.
Then it happens that later any one or combination of these sensory factors can re-stimulate the same state of consciousness as the original event, and so re-trigger the memory. This is what a re-triggering is. So we could say as part of a definition of re-traumatisation that:
Re-traumatisation is the state-dependent re-triggering of a memory that was traumatic.
However Rossi goes on to say that the re-stimulated memory, instead of being a pure repetition of the original event can become a healing experience if the person is aware of some component in the present that is different from the original event, and is experienced as safe and supportive, ie the supportive presence of the therapist.
According to Rossi this replaces the original state of consciousness with a new 'improved' state of consciousness. So if the memory is re-triggered again at some point in the future, part of the state dependent memory includes this new experiential component. In neuorological terms this experience of the new element will create new neurological connections and is the process of neuroplasticity, that then remains as a new, updated version.
Neuroplasticity: The brain's ability to reorganize itself by forming new neural connections throughout life. Neuroplasticity allows the neurons (nerve cells) in the brain to compensate for injury and disease and to adjust their activities in response to new situations or to changes in their environment. Wikipedia
Current attitudes towards re-traumatisation
Currently there is a lot of fear around this topic, which comes, in my view, from a lack of openness, exploration, discussion and good information.
The tendency now I think is to try and avoid an incidence of re-traumatisation at all costs, a kind of, in my view unrealistic, rigid protectionism, which leads to a perspective that if one is a good therapist-facilitator it doesn’t/shouldn’t happen.
Then if it does happen this leads to criticism and disapprobation towards the facilitator, thereby causing shame, leading to a culture of secrecy and further lack of open discussion and exploration of the topic, and so on.
The first thing I want to say to all practitioners is: in your practice as a trauma therapist it is inevitable that people, whether client or representative, will have state-dependent traumatic memories re-stimulated. Most often this is in the form of a re-triggering that their survival strategies can deal with, rather than a full re-traumatisation. In my view if we are working with trauma this is not avoidable.
As stated above, if it is a re-triggering this can usually be managed by the person's own survival strategies. What follows focuses on the situation when the person's survival strategies fail and they go into a full and helpless re-traumatisation.
Three questions to consider
The three vital questions that follow are:
- How can we recognise the onset of re-traumatisation?
- How might we interrupt the process usefully and respectfully?
- If the person goes into a full re-traumatisation what can we then do to turn it into a helpful, even transformative, experience rather than an unhelpful experience for the person, and for the group?
How to recognise the onset of re-traumatisation
The recognition of the onset of re-traumatisation is the same whether the person is the client, a representative, or an observing member of the group. However I will just say something about the representative situation first.
The Representative Experience: We know from our experiences as facilitator-therapists working with the Intention Method (or even from prior experiences of working with family constellations) that representatives uncannily are often chosen to represent elements/people that involve similar past experiences to their own. This inevitable concurrence in my view is useful in the work as, at its most satisfying, it can mean that the work of the client becomes productive for others at the same time. But it can also be a route to re-traumatisation.
Most commonly the representative experience is a meta- or concurrent resonance experience, where the connection with oneself remains in tact. I tend to think that it is a kind of 60%/40% balance of representation/actual person (healthy self). However, if the representative gets lost in the experience of their representation, to the extent that they lose contact with their healthy self, they are then likely to be re-triggered into their own trauma by their representation.
The main recognition points for any onset of re-traumatisation:
- Body shaking, legs trembling, any kind of tremoring: This is a primary Red Flag and a visible sign. These are signs that the physical body is coming under extreme stress from holding the trauma as it rises to expression...
- Look of panic/dissociation, rapid breathing, blank look in the eyes: This is a primary Red Flag and a visible sign. The person obviously seems to be losing contact with what is happening in the present and is in panic.
- Eyes consistently closed: This is a primary Red Flag, but might be confusing. My questions to myself as facilitator would be: where are they in their internal world? Are they aware of the present context or are they transported back to an earlier, traumatising context? Sometimes people close their eyes to get more in contact with their experience… this would not be a re-traumatising situation. But if they remain with their eyes closed for a long time, and seem not to have much contact with what is going on around them this might be the onset of re-traumatisation. Solution: just ask… say their name and ask them to look at you so that you can be confident they know where they are. If they are fine they will say so and look at you and you will have a sense of contact with them; if they still do not open their eyes, or if they do and look at you but you do not experience it as being proper contact with you (ie their look is dissociated) you can then take necessary steps (see below).
- Expression of strong emotions by a representative: If the person as a representative is going into strong emotions your question to yourself should be: are these really the emotions that belong to the client, or is this person getting lost in their own trauma emotions? Solution: Again, you can say their name and get some contact… then you will know. In my view in the overall work emotions that belong to the client, especially strong emotions, will at some point need to be experienced by the client… not the representative. Very often what we see in a representation is that the representative will touch into some strong emotions as a way of indicating the existence of the emotions to the client, but have the ability to come out if spoken to… but if they really start to express deep, strong emotions that might be a point at which you want to check.
- Expression of strong emotions by the client: this is usually fine, and often is a relief and a release for the representatives in the work, and they may go to the client and hold her/him while she/he expresses the emotions. So long as you feel confident that the client knows where he/she is and is aware of the present supportive contact and situation all should be okay. After all, in the end this is what our work is about, the expression of long suppressed emotions. Just stay alert and watch to make sure the person continues to know where they are and is aware of those around them.
Representatives who are just being representatives can always respond to a question from the facilitator-therapist… they are able to go in and come out of the role reasonably easily. Representatives who do not do that easily you might need to keep a conscious eye on.
If a full re-traumatisation occurs…
What to do if you are faced with someone going helplessly into a full, potentially unhelpful, re-traumatisation?
The general approach is to ensure that they maintain contact with the here and now reality… personified by the clear, supportive presence of the therapist.
- Stay in your healthy self and don’t panic.
- Stop the work. If the client is not psychologically present (ie sufficiently in their healthy self) there is no point in continuing the work. The point of the work is that the client gains something from it, and if they can't there is no point.
- Speak in a clear, calm everyday voice… do not speak too softly or in a gentle voice… this can be experienced as hypnotic and in their state they are already likely to be in a severely hypnotic and dissociated state. So speak clearly and with reasonable volume.
- Address the person by name and ask them to open their eyes
- If they do open their eyes make sure that they see you, that you have contact with them, that they know who you are and that you are there. Keep talking to them clearly and calmly... keep the contact.
- If they do not open their eyes keep talking to them until they do. They will know you are there by the sound of your voice, so keep talking in a calm way. Perhaps ask if they can hear you. Any question that requires an answer will help them to come more into contact with you. We are conditioned to answer questions!
- Stand in front of them if you can, so that when they open their eyes they can clearly see who you are and not mistake you for someone else, but not so close that when they open their eyes you are experienced as a threat or are out of focus for them.
- If you feel okay to do so, touch them in a clear way, perhaps on the shoulder, or take their hand. Physical contact helps them maintain a connection with the here and now through their body. It might be helpful to say first that you are going to take their hand or touch them on the shoulder as a way of anchoring them in the present...
- Keep talking until you are clear that they know where they are. Reassure them that you are there and you are going to remain with them until they are fully okay.
- In severe cases if their eyes are open but seem not to connect with anything you can ask them to describe the surroundings, colours, furniture, people etc.
- You can also suggest they regulate their breathing (particularly if they are hyperventilating... panic breathing - see below)
- You can suggest they come into contact with their body... "Do you feel the ground beneath your feet?", "Do you feel the chair you are sitting on?", "How does your body feel?", "Can you feel your hands/feet/legs?"
- Once you are sure you have contact with them you can then stay with them while they experience/express the trauma emotions and, if you feel okay to do so, hold them while they do this. You can ask them if they would like you to hold them (another question... requiring an answer).
- Trauma expression involves strong feelings and may also involve physical shaking and trembling… let this happen. It is quite safe providing you are sure that they know where they are and who you are, that you can maintain contact with them.
- Do not rush the process; stay with them until you are both quite sure that the person is fully back in the present and reasonably in touch with their healthy self.
- Leave sufficient time for the group to do or say whatever they need to about what has happened, to process it.
In most situations these strategies are sufficient, and helpful. As one client in a group said to me "This experience was so different because you were there. In the original situation there was no one." That is the up-grading of the state dependent memory.
A note about hyperventilation:
Panic causes hyperventilation... accelerated, over fast breathing accompanied by rapid heartbeat, and the symptoms of hyperventilation can cause the person to feel increased panic, especially if they do not understand what is happening.
The most important thing to understand about hyperventilation is that although it can feel as if you don’t have enough oxygen - hence the attempt to increase breathing - in fact the opposite is true. It is a symptom of too much oxygen and a lack of carbon dioxide. After a while this causes dizziness and an unpleasant feeling of numbness in the extremities (hands and feet). It can also cause chest pains and other symptoms. If the person says that they are feeling dizzy or any other unusual physical symptoms just tell them that they are hyper-ventilating... it isn't dangerous and see if they can hold their breath for a short time and then regulate their breathing, or see if they can take their breath deep down into their abdomen rather than the shallow, upper chest breathing that is hyperventilation. Keep reassuring them and encouraging them to regulate their breathing until it is better regulated.
Psychosis
On the rare occasion that these strategies are not sufficient and you cannot find a way of keeping the person in contact with the present reality, it is possible that they are going into psychosis and you may need to get further help. Keep talking to them and keep trying to get them grounded and in the present as best you can while you wait for help. So in a group setting you might ask if anyone in the group is a doctor or for some other more formal help. However it is unlikely that you will be unable to have some contact with the person and may even be able to discuss with them what might be the best next steps.
In my nearly 20 years of working with the constellations/representation method this has only happened once, and in that situation the person had had previous psychotic episodes and knew what was happening… he understood the signs… and knew precisely what to do… he went and checked himself into a familiar psychiatric unit without my help, informing me that that was what he was going to do. I kept in reasonable contact with the authorities and with him as a reassurance to myself, and to him, that just because he had gone into psychiatric care I still maintained an awareness of him.
It is useful to remember that psychosis in itself is a survival impulse... and that even in a psychotic state there still exists a healthy self and you may be able to contact it.
Why might a re-traumatisation happen?
In the end the purpose of the work for the client is that they express the unexpressed trauma emotions in the safe context of the controlled working environment. There are of course many steps to this, and much of the work for the client will be the business of recognising and familiarising themselves with their survival strategies, thereby strengthening their healthy self and gaining access to the truth of their history and biography. Theoretically we cannot safely approach our traumatised self until we have sufficient connection with our strengthened healthy self. However along the way there are always moments when the client will be able to express some of the trauma feelings. This is a healthy process.
In my view incidents of severe re-traumatisation within the work environment are probably always caused by a mistake or mishandling on the part of the facilitator. We all make mistakes, and particularly while we are learning how to work as a facilitator. It is a paradoxical situation: you cannot learn how to be a competent facilitator without gaining practical experience, and at the same time while gaining the practical experience one must make mistakes! It is a truism that we learn from and remember best our mistakes and what they teach us.
In my view there are several things that the facilitator might do that could contribute to such a mishandling, but rather than list these I am going to list those things that I think we must hold onto in our work that help keep us and our clients and representatives in contact with their healthy self:
- Stay consciously in your healthy self as much as you can, and know your own survival strategies and triggers well enough to be able to know in the present moment if you lose your healthy stance. Do not carry on facilitating if you are in your survival self... you too have vulnerabilities... and rights. Be honest... the participants will respect you for your honesty and your respect for yourself and your limits.
- Stay in touch with the client, always. Do not get more involved in what the representatives are doing than in your connection with the client. This is a classic situation in which a client might get re-traumatised, when the therapist loses touch with what is happening for the client and is too much occupied with the representations.
- At the same time do keep an eye on the representatives... just in case.
- Trust the client. Trust their healthy self, but also trust and respect their survival self… do not push them if they go into survival, instead see that this is a clear message that they are at their edge. This is another classic mistake which can cause re-traumatisation... where the facilitator overrides or ignores the survival impulses of the client.
- Do not let the work go on too long if it is an obvious survival intention. As you continue your learning you will come to know those intentions that are more designed to confuse and distract than to get to the point. Continuing with the work with such an intention for too long is also pushing against the survival instincts of the client. Their distractive and confusing intention is there for a good reason.
- Keep on the safer side… If you feel uncertain about whether a representative is getting in too deep simply remind them that they are ‘just a representative’… better to keep on the safer side than not.
- If you feel ashamed about anything go and do your own personal work. There is nothing to be ashamed of. We all make mistakes, we are all learning and we are all doing our best.
Do please contribute to this paper in the comments section… I have put down everything I can think of about this topic at the moment, but I am quite sure there is more…
References
Broughton, V. (2016). Becoming Your True Self: A handbook for the journey from trauma to healthy autonomy. Green Balloon Publishing, Steyning, UK.
Broughton, V. (2013). The Heart of Things: Understanding Trauma – Working with Constellations. Green Balloon Publishing, Steyning, UK.
Cheek, David B. & Rossi, E. (1995) Mind-Body Therapy: Methods of Ideodynamic healing in Hypnosis
Lewis, T., Amini, F. & Lannon, R. (2001). A General Theory of Love. Vintage Books, New York.
Rizzolatti, G. & Craighero, L. (2004). The Mirror-Neruon System, in Annual Review of Neuroscience, 27.
Ruppert, F. Trauma, Fear & Love: How the Constellation of the Intention Supports Healthy Autonomy. Green Balloon Publishing, Steyning, UK.
Siegel, D. J., (2010). The Mindful Therapist: A Clinician’s Guide to Mindsight and Neural Integration. Norton Publishing, New York.

Write a comment
Tina (Saturday, 31 October 2020 19:53)
I found your explanations of the splitting process very insightful!
For the part on "Why might a re-traumatisation happen?" and especially your suggestions how to keep the client safe some examples would have helped me enormously to really understand what in practice it means.
Vivian Broughton (Sunday, 01 November 2020 09:59)
Yes I understand what you are saying... thank you for the feedback.
best wishes
Gabriela (Thursday, 31 March 2022 21:53)
This article is extremely helpful. I especially appreciate that you speak about retraumatisation, because in my eyes this topic continues being a taboo and it shouldn't. Thank you.
Vivian Broughton (Tuesday, 05 April 2022 12:05)
thank you for your feedback... and yes, any kind of therapeutic practitioner must understand the reality of retraumatisation, otherwise it will happen and not be understood. It is dangerous for any therapeutic practitioner to think that this will not happen in their work...
Go well.